- Posted By: Dr.aya noaman
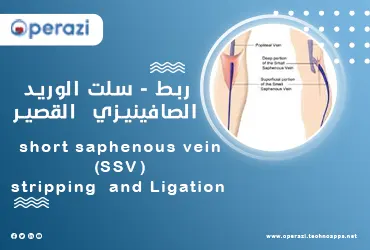
short saphenous vein (SSV) stripping and Ligation is a surgical procedure we use to remove severely damaged veins in the legs, which are causing venous insufficiency or varicose veins. Once the damaged vein is removed, it will take over other veins in your body to allow blood to flow in that part of your leg. Our Cardiovascular Services at operazi offer the latest innovations in vascular care for patients. operazi can perform the short saphenous vein (SSV) stripping and Ligation in installments. For our services, click here.
Who is a Candidate for short saphenous vein (SSV) stripping and Ligation?
You good candidate if you:
• They have severe venous insufficiency.
• They have very large varicose veins.
• Are at risk of developing venous ulcers or already have skin ulcers.
• You experience frequent pain or heaviness in your legs.
• You have severe leg pain.
• Damaged veins in places where superficial veins (closest to the surface of the skin) connect to deep veins.
A vascular surgeon may discuss other options instead of surgery if you:
• Older.
• You have other medical conditions that put you at greater risk of complications from the surgery.
• You have poor blood circulation in the arteries in your leg (the large blood vessels that carry oxygen from your heart to your body).
• You have swelling or fluid buildup in the area of the varicose veins due to lymphedema.
• You have a skin infection.
• They are more prone to blood clots.
•pregnant.
We at operazi offer both surgical and non-surgical treatment options to help you customize the treatment plan that best suits your needs.
See also: surgical prostatectomy
What do you expect on your first date with operazi?
At your first appointment, you'll meet with a vascular surgeon who will ask about your medical history and discuss your concerns about venous insufficiency and/or varicose veins. They will examine your legs and look for other symptoms, such as swelling, discoloration of the skin or varicose veins. Any invisible symptoms, such as itching or pain, should also be discussed with your provider.
We may order an ultrasound to see what's going on inside your veins. We'll run a small hand-held device (called a transducer) over the top of your skin to see pictures of the veins inside your legs. These ultrasound images will help us create the best treatment plan for you, also you can search for a vascular surgeon in operazi
How do you prepare for a short saphenous vein (SSV) stripping and Ligation surgery?
Vein ligation and stripping is a minor surgery. You will sleep under general anesthesia. It is important to follow your surgeon's instructions to prepare for surgery.
• You will not be able to drive on your own after you are out of anaesthesia.
• Your surgeon and anesthesiologist will meet with you before surgery to discuss the procedure and answer any questions you have.
What happens during a short saphenous vein (SSV) stripping and Ligation surgery?
• The vascular surgeon will make two small incisions (incisions) - one in the groin area (near the top of the damaged vein) and one in the thigh or calf (below the vein).
• The surgeon will tie off the upper part of the vein to stop the blood flow. A thin, flexible device will be passed through the damaged vein. The surgeon will use the device to pull the entire vein out through an incision (cut) below the vein.
Once the vein is removed, the surgeon will stitch up your incisions and place dressings over them. This procedure is called phlebectomy or microdissection and can be done at the same time as vein stripping and ligation.
After surgery is complete, your surgeon will place gauze and an ACE-compression roll on your treated leg. You will be taken to the recovery room to rest and wake up from the anesthesia. You'll be in the recovery room for one to two hours before a family member or friend can take you home. The surgeon will give you compression stockings to wear the next day after the dressings are taken off, and our vascular surgeons in operazi can treat all types of conditions that lead to venous insufficiency and varicose veins.
Complications of ligation of the short saphenous vein
The most common risks include:
• Infection after surgery.
• Bleeding.
• Blood clots.
• Scarring or bruising at the site of surgery.
• Injury to the nerves around the vein.
• reaction to anesthesia.
Recovery time with short saphenous vein (SSV) stripping and Ligation surgery
You will need to wear compression stockings for about two to four weeks after surgery for your leg to recover. Healing time may vary depending on the number and location of the veins stripped. Your surgeon will discuss the healing process with you in more detail.
Signs of recovery after surgery
• You may feel some slight pain after the vein ligation and stripping surgery. If necessary, you can take over-the-counter pain relievers to control the pain. Your pain will improve as your legs heal.
• Most people experience significant bruising immediately after surgery. Postoperative bruising takes up to three weeks to heal.
• It will take about three weeks for your incisions to heal and the stitches to dissolve.
Bathing and showering after surgery
• Don't shower until your doctor tells you can take off your bandages and compression stockings, usually the day after surgery.
See also: drainage of renal abcess
Resume daily activities
Most people will be able to get around within a few hours after surgery. As your legs recover over the next two to four weeks, continue to elevate your legs as much as you can while sitting.
It's important to move your legs and keep blood flowing as much as possible once your surgeon has authorized you to resume normal activity. We suggest you:
• Walk around once every hour for 10 to 15 minutes at a time.
• Flex and direct your feet while sitting or lying down.
• Increase your intake of exercise each day as your legs begin to feel better and the cracks (wounds) heal.
Do not do any strenuous exercise such as lifting heavy objects until your surgeon tells you to do so safely.
Driving and back to work
You will not be able to drive for at least three days. Talk to your doctor about when you can resume driving. Most people can return to work one week after recovery. If your job involves physical stress, standing for long periods of time, or other activities that can put pressure on your legs, your doctor may tell you to wait longer before returning to work.
;